I am Saranya ,a final
year MBBS student.
Greetings to all my readers;
This is an elog documenting the patients that I
witness during my Clinical Postings to enforce a greater patient centered
learning .
DEIDENTIFICATION :
The privacy of the patient is being entirely
conserved. No identifiers shall be revealed through out the piece of work
whatsoever.
Introduction :
Here we shall discuss about
a patient who is a 45 year old farmer hailing from South India .
PRESENTING
PICTURE OF THE PATIENT :
Day 1
The patient
presented to the OPD with complaints of
-Fever
since 4 days
-Body
pains since 3 days
-Reduced
urine since 2 days
-Vomiting
yesterday
-Black
stools since morning
Please
note : Patient was hypotension (70/40 mm Hg B.p was recorded ) on presentation and he was agitated, dyspneic ,was
complaining of headache and was thirsty
Sequence
of events which led to the presentation of the patient :
Patient
is a farmer hence works in the farm from morning till eve, until 4 days back ( 29th
October 2021 ) when he developed fever along with cough ,headache. He received medications
given by the local physician but nothing much changed
A day
or two later he developed muscle pains which he described to be in both his arms
and thighs and the fever was back again
He took
medications for one more day
But nothing
seemed to improve
Also
a new addition to his problems were vomiting
This
was when he was taken to Hospital1 where the attenders gave information about the patient being given
fluids but they felt that proper care was not being taken and hence they brought
the patient to Hospital2
When
we asked more questions, we found out that he had passed much less urine than he
usually does since the past couple of days and that day he had passed stools which
were black in colour.
Daily Routine of the patient :
He normally
used to get up at 5.00 am ,freshen up and go to the fields , in the afternoon at
around 1.30pm he would return home for lunch, post which he took rest for an hour,
by this time it would be around 3.00 pm
He would
again go out for work for another 2 hours and then return home , take a bath ,have
his meal .Many a times he would go out to drink alcohol in the evenings. After spending
an hour or so talking to his wife and two sons over the meal
And then
he would sleep by 9.00 pm.
Some
more details about his complaints
High
grade fever , intermittent and not associated with chills and rigors .
H/o
2 episodes of non projectile, non bilious, blood tinged vomiting
yesterday
-Hematuria
since morning
-1
episode of black tarry stool in the morning
-Reduced
urine output since morning
Addictions
:
He
is an alcoholic since the past 20 years with around 90 ml of whiskey everyday.
His last intake of whiskey was 4 days. He smokes around 2 packs of beedi
everyday since the past 20 years.
GENERAL
EXAMINATION :
PR -
118 bpm
BP- 70 /40 mm Hg ( started on fluids and ionotropes)
RR -
25 cpm
Spo2
- 92% on Room air
Afebrile
Lungs
-
Inspiratory
crepitations in Bilteral IAA,ISA
Cvs
- S1,S2+
Per
Abdomen -
Soft
Nontender
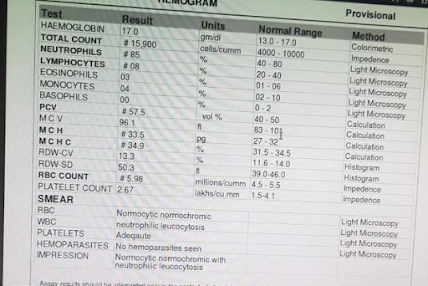
HB -
8 ( outside 2 days back 11g/dl)
TLC
- 8400
Plt
- 15,000
Total
Bilirubin - 11
Direct
Bil - 7.05
Ast
- 327
Alt
- 187
Alp
- 303
Albumin
- 2.4
Serum
creatinine - 2.5
NOTE : There is history of change in water source and also contamination of right ankle with rat's urine in his farmlands
Some
textbook description of Weil's Disease :
Courtesy
declaration: The following images are not original and have
been taken for reference from the below mentioned source .
Source : Davidson's Principles and Practice of Medicine
23rd
Edition
Infectious
Diseases
Note : On 5th November 2021 evening ,patient developed Cardiac Arrest owing to the Myocarditis entity and was revived by cardiopulmonary resuscitation.
UPDATE :8th November 2021
http://prashanthsharma101.blogspot.com/2021/11/case-of-45-years-old-man.html
Patient is having fever spikes , cough with sputum yellow coloured,non blood stained ,shortness of breath , generalized bodypains .
Yesterday night - patient had one episode of high grade fever with chills ,became tachypneic .
Connected to NIV - CPAP.
ABG with high flow oxygen showed Hypoxia ,hence
Patient was on CPAP PC mode overnight
With RR- 33/ min
Peep - 7
Fio2-50%
icteric,pallor, subconjunctival hemorrhage
Afebrile
PR-90/ min ,regular
BP- 130/90 mmhg
RR-37 / min
Spo2- 100% with fio2-80%
RS- BAE present ,bilateral crepts + infraxillary ,infrascpular regions .
CvS- S1,S2 heard
P/ A soft
1-MODS- weils syndrome
2- Ventilator Associated pneumonia ?
Iv fluids
Inj . ceftriaxone 1gm / IV/BD
Inj.doxy 100 mg / IV/BD
TEMP charting ,vitals monitoring.
In view of persistent fever spikes ,hypoxia , tachypnea,new radiological opacties -Emperical antibiotic coverage for VAP was started with levofloxacin and vancomycin .