EXPECTATION FROM THIS E LOG :
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I thank Dr. Chitra , for providing me with every detail about the patient , and also being extremely patient with my doubts about the case.
Introduction :
The Patient is a 27 year old Male , a Post Office Employee in Telangana .
Chief Complaint :
The Patient presented to the Casualty on 5th June 2021 with complaints of Pain in Upper Abdomen since the morning of that day.
History of Presenting Illness :
( Certain Past Events shall also be mentioned here , if they have a role in the present manifestation of the pathology )
The patient has been an Alcoholic since 5 years , with a daily intake of about 180 ml of Whiskey .
The Patient developed pain in the Upper Abdomen in the early morning hours of 5th June 2021 and was rushed to the hospital.
Pain was sudden in onset , rapidly progressing , aggravated ( burning sensation ) by spicy/heavy food intake , no relieving factors as such.
He described the pain to be diffuse , radiating to the back .
Not associated with
Nausea/ Vomiting
Shoulder Tip Pain
Distended Abdomen.
Last History of Alcohol Intake : 2nd June 2021
Past History :
No similar Complaints of Acute Abdominal Pain in the past,.
In 2014, he had had an acute attack of SOB,triggered by cold exposure , had got relieved on medication .
He was prescribed Inhalers but is not compliant to the same.
In 2015, he had an episode of Epilepsy , for which he is under medication .
He is not a K/C/O DM , HTM , CAD .
Personal History :
Appetite is normal ,
Takes Mixed Diet,
Bowel and Bladder : Normal
Sleep : Adequate
Does not Smoke
Is a Regular Alcoholic since 5 years ( details mentioned above )
No known food or drug allergies .
He is less tolerant to cold exposure / cold food/drinks . (Asthma Trigger )
Family History :
Not Significant.
Treatment History :
Has had a Surgical repair for Inguinal Hernia 4 years ago.
NOTES :
EXAMINATION :
GENERAL EXAMINATION :
The patient was examined in both sitting and supine position after obtaining Consent . Examination was done in a well lit room , in the presence of an attendant , with adequate exposure .
Patient in Pain .Wincing Expression . ( Wong Baker's Rating : 8 ) .
Patient is not still on bed.
The patient is of moderate nutrition and built.
TRUNCAL OBESITY PRESENT.
Conscious , Coherent , Cooperative . Oriented to time , place and person.
He does not have
Pallor, Icterus , Cyanosis , Koilonychia , Clubbing ,Generalised Lymphadenopathy ,Pedal Edema.
VITALS on Presentation :
Pulse : 110 bpm , normal Rythm , volume , condition of vessel wall , without any delay.
B.p : 130 / 80 mm Hg recorded in the Right Brachial Artery in supine position
R.R : 22 cpm
Body Temp. : Afebrile .
SpO2 : 98 % on r.a.
Pain : Present , Rating 8 ( Wong Bakers Rating ).
SYSTEMIC EXAMINATION :
CVS : normal
RESPIRATORY SYSTEM : normal
CNS : normal
ABDOMEN : Abdomen soft , tender.
Note : Tender Abdomen .Abdomen is distension has increased . On 6/June/2021 night : Resonant note was obtained up to 3 cm above the umblicus but
On 7/jun/2021 morning : Resonant notes percieved till below the umblicus.
Shifting Dullness present .
INVESTIGATIONS :
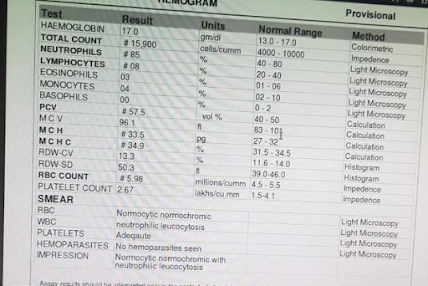
Complete Blood Count
Urine Sample
COMPLETE URINE EXAMINATION
COAGULATION PROFILE :
LDH raised
SERUM LIPASE raised
SERUM AMYLASE raised
Normal Random Blood GLucose
LFT
CHEST RADIOGRAPH
RYLE'S TUBE ASPIRATE.
FEVER CHART
CROSS CONSULTATION NOTES :
Provisional Diagnosis : A 27 year old man , chronic alcoholic with acute pancreatitis and Grade II Steatohepatitis .
INTERVENTIONS DONE :
Plan of Management : Conservative.
Communication with Attenders : Outcome has been adequately explained .
Medications :
UPDATED : ( 9th June 2021 )
i


























No comments:
Post a Comment